How Diet Affects Mood
Is what you’re eating affecting your body besides just your stomach?
The human body is a walking colony for millions of microorganisms that help us function, but the stomach and intestines are the most populated organs that have an entire mini ecosystem of their own, known collectively as the gut microbiome. While most of us just eat based on what’s available or based on our preferences, the latest research in the scientific field suggests that our gut microbiome and what we feed it has major negative impacts on our brain.
According to Heathline’s article on the topic, the microbiome consists of various species of bacteria that serve different purposes, including aiding in digestion, regulating the immune system, protecting against harmful bacteria, and producing some beneficial vitamins. It can actually impact other aspects of the body, such as the heart, a person’s weight, and even their internal temperature, but those are typically balanced so that a person is healthy. The effects on the brain, however, are not physically regulated by the body as the other parts are, and this is what leads to changes in mood, anxiety, and depression.
The gut microbiome, which consists of the stomach and intestines, is home to trillions of microorganisms.
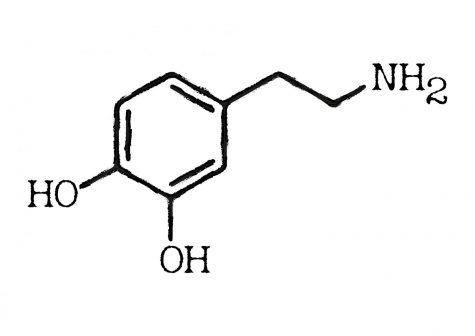
A related Healthline article discussed some of the side effects of an unhealthy gut microbiome, including serotonin deficiency. Serotonin is an antidepressant neurotransmitter (a chemical that travels through the nerves) that is mostly produced in the stomach, so having an unhealthy gut microbiome means a lower count of serotonin is being produced. This, in turn, can cause anxiety, depression, aggression, impulsive behavior, insomnia, irritability, low self-esteem, poor appetite, and poor memory. Serotonin deficiency leads to physical symptoms, and it has even been linked to psychological disorders.
Science writer Elizabeth Pennisi explains in her article, Evidence mounts that gut bacteria can influence mood, prevent depression, on AAAS, how this research came to be and what it means. The connections between the gut microbiome and the brain were originally discovered through experiments on mice, but observations and tests in humans were soon conducted. Along with his colleagues, Jereon Raes, a microbiologist at the Catholic University of Leuven in Belgium, conducted a series of tests that compared the microbiomes of people who were healthy and had higher quality lives to people who were diagnosed with depression or had poorer quality lives. The tests found that the people who had depression were missing two different kinds of microbes: Coprococcus and Dialister. The researchers even tested the theory including variables such as age, sex, and antidepressant use, and found that the results were the same, despite the fact that those variables all affect the gut microbiome differently. At the same time, the people who had been diagnosed with depression had a large population of bacteria associated with Crohn disease, which is inflammation of the bowels, and many of them had said inflammation.
While the conclusions were solid, the research by Raes was only on one sample population, and the gut microbiome in a sample population differs from the rest of the world due to diet, air, and lifestyle. However, the research team compared their data with a sample of 1064 Dutch people who had also been tested, and they found that the results were the same, solidifying the accuracy of their data.
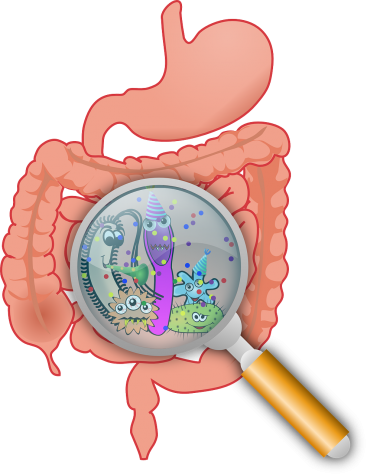
It is not just serotonin that is not being produced in the unhealthy gut microbiomes. The Coprococcus bacteria missing from the unhealthy samples also seemed to be responsible, in part, for the production of dopamine, which is a vital hormone for happiness and gratification. As a result, a lower amount of dopamine aids depression. Not only that, but Coprococcus is also responsible for producing butyrate, which is an anti-inflammatory substance, and people with depression tend to have inflammation in the digestive tract. This inflammation actually connects back to the increase in bacteria found in Crohn disease stated before.
The chemical structure of dopamine, which is responsible for the brain’s feeling of satisfaction.
The results are undeniable: the gut microbiome can affect the brain and mood. However, the exact “how” of the data is still theoretical and being researched. It is clear that the gut microbiome is affecting the brain due to an absence of certain species of bacteria and microbes, but how it is doing so is still unknown. One possibility is that the chemicals produced in the stomach and sent to the brain through the vagus nerve, which links the brain and the gut, is not occurring, resulting in a lower supply of dopamine and serotonin as stated before.
The “how” is essential for creating therapeutic measures to counter the negative effects, although companies have already begun to work on solving that problem. Probiotics are one solution that are already available, but due to how new the research is, the probiotics depressed people are taking do not contain the necessary bacteria that have been found to be missing from the gut. A newer therapy is the concept of fecal transplants, and research regarding this theory has already begun with clinical trials already underway. The fecal transplant works by having a sample of fecal matter of a healthy patient injected into the intestines of an unhealthy patient. The healthy sample contains the bacteria and microbes that are missing in the gut microbiome of the unhealthy patient, and from the injection, they will begin to repopulate, and eventually, the unhealthy patient’s microbiome will be restored.
The research is new and still has a long way to go, but the findings have opened up a new field of therapies, symptom identification, and explanations for patterns in the human brian. Mentioned in Pennisi’s article, Sven Pettersson, an experimental biologist at the Karolinska Institute in Stockholm, believes that the research should be a signal to the clinical community to start profiling patients with mental illnesses by their gut microbiomes. In other words, the medical world might be able to identify and cure patients with mental illnesses based on the health of their gut microbiome and which bacteria and microbe populations are high or low in them.

A healthy balanced diet is important for maintaining a good gut microbiome.
So, what does this mean for everyone not in the scientific or medical field? Well, it means that your diet could be affecting your mood and brain in ways that you never realized. The best way to counter these negative effects: make sure to eat a healthy, balanced diet, and especially be sure to avoid antibiotics as best as you can. Both can help or harm the bacteria and microbes in your body. For a thorough, in-depth plan to keep your gut microbiome healthy, be sure to check out Clean Eating’s article about eight easy steps you can take to keep your gut microbiome happy and healthy.

Vince is a senior at LRHS and a prominent staff writer for The Lancer Ledger. He has been a dedicated writer for over two years straight, devoting most...